OpEds
Like walking in three feet of snow with no end in sight
We are now well into a third wave of COVID-19, and it seems we are still a few weeks away from its peak. All evidence suggests that this surge of infections will outnumber those of the waves we have already endured. By now, we all have friends and family who have suffered and sadly succumbed to this pandemic, and it feels like it’s hitting ever closer to home.
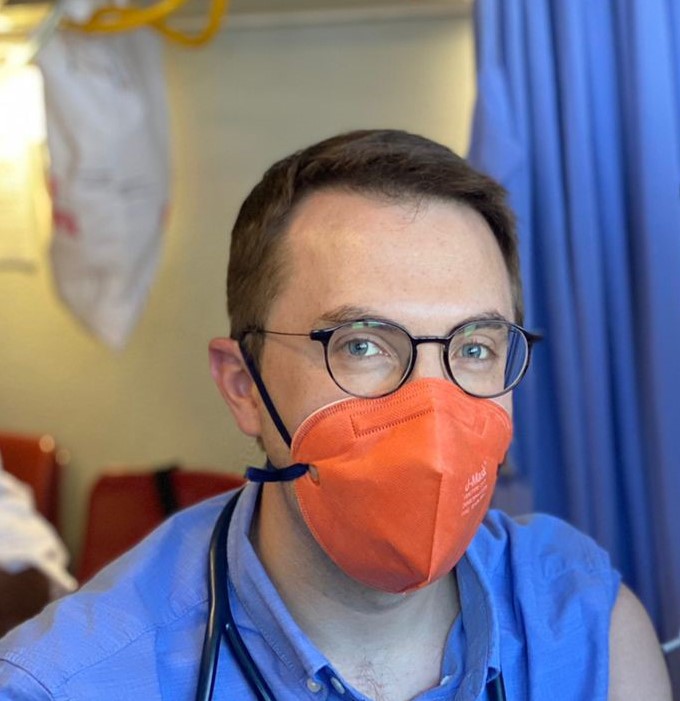
I work at a large state tertiary healthcare facility. As a consultant specialist physician, I work with patients infected with COVID-19 spanning the full spectrum of severity of illness, including being responsible for the care of critically ill and ventilated patients. I have experienced this pandemic first hand from its start from the perspective of a friend, relative, community member, and frontline worker. The devastation this virus has caused on all fronts is unparalleled.
It seems like each wave has brought with it its own set of unique challenges and heartbreaks. I remember vividly the feelings of trepidation and nervousness we all felt waiting for the inevitable first wave to arrive. The initial hard lockdown, while difficult to endure, doubtless saved many lives by delaying the surge, giving us time to prepare for what would come.
When the first cases came, we still weren’t sure what strategies would work best in our setting, and we had to learn from experience. The influx of patients quickly overwhelmed our relatively small department, and we required the support of health professionals from other disciplines to assist us to cope with the load.
During the surges, we still make use of physician-led teams and work alongside orthopaedic surgeons, anaesthesiologists, neurosurgeons, and doctors from many other disciplines. Many are young medical officers and registrars. I’m constantly in awe at how resilient and optimistic they remain in the face of such adversity.
When the second wave hit, I watched how the intensive-care unit went from almost empty to full in just a matter of days. I remember the despair we felt that a new wave had come seemingly so soon after barely enough time had elapsed to recover from the first.
This third wave is again different. The speed and severity with which it has spread in our community has been hard to bear. Almost every day, I have been informed about someone infected, in need of hospitalisation, or sadly of those who have succumbed to their illness.
The devastation is all the more heart breaking this time around because we know that the vaccination rollout that could have prevented so much heartbreak is coming too late for many.
However, all hope isn’t lost. We know without doubt that social distancing, rigorous hand hygiene, and wearing of masks prevents the spread of infection. We know that the vaccination is safe and effective.
We have also gained tremendous insight into the care of patients infected with COVID-19, and have successfully discharged many who may not have been so fortunate at the start of the pandemic. We have very clear reasons to remain optimistic.
What has limited our success has been an inability to provide suitable care in a timely manner to many of our patients. During these surges of infection, our resources rapidly become overwhelmed, which results in significant limitations in accessing care. Working in an already resource-limited sector, we are again in a position where critical-care beds need to be triaged and given to patients with the best predicted outcomes.
This means, sadly, that not all of our patients will ultimately have access to potentially lifesaving care. Unfortunately, the ongoing closure of Charlotte Maxeke Johannesburg Academic Hospital and the troubles facing other state facilities in our referral area have exacerbated the problem.
By now, most private hospitals have reached capacity too, and are looking elsewhere for assistance. I often get called by private facilities seeking to help patients needing critical-care admission. In our current climate, having a medical aid does not imply an easy access to a necessary level of care.
Compounding the problem is ever worsening staff fatigue. Critical-care nursing is highly specialised and the shortage of trained personnel in all sectors has resulted in these individuals, as well as other healthcare professionals including physiotherapists, dieticians, radiographers, medical technologists, and others, extending themselves significantly. Burnout is high, and staff are tired. To quote a senior medical colleague, “It feels like walking in three feet of snow, with no end in sight. One foot in front of the other, on and on and on.”
Several facilities now offer post-COVID-19 clinics, where discharged patients can go for post-hospital COVID-19 support.
Beyond debilitating physical after effects, many patients experience ongoing fatigue, anxiety and mental illness after their acute illness has passed. Many watched others suffer or die and thought that they themselves may die too. Our patients are isolated from the outside world, isolated from their families and do not know if they will ever return to them. These wounds take a long time to heal.
It’s self-evident how quickly resources become consumed and overwhelmed during surges such as this one. The rapidity with which critical-care services in particular are required and depleted during a wave of infection makes this virus distinctly dangerous.
It’s also clear that anyone is at risk from infection. I have seen people succumb to infection at a young age, without risk factors. Even in our survivors, I have seen young patients left disabled by their infection, left with symptoms that impair their ability to work and conduct themselves as they would have prior to infection.
Finally, a considerable amount of data now exists, garnered from rigorous scientific method, that shows vaccination to be effective and safe. The only way to reduce transmission and severity of COVID-19 infection is through vaccination.
I have no doubt we will overcome this wave and any waves that follow. Sadly, whatever successes we have now and in the future will always be overridden by the devastation felt by all of us who have lost friends, colleagues, and loved ones.
I urge everyone to do whatever you can to prevent the spread of infection in our community. Adhere to the advice of experts, follow the rules, and get vaccinated as soon as it’s available.
If you have the means, please support our communal institutions, they are doing amazing work and need our support now more than ever.
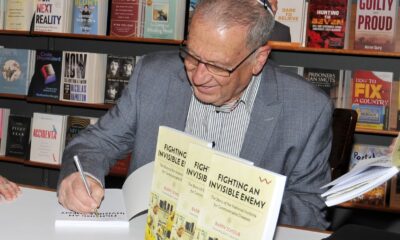
- Dr Darren Joseph is a specialist physician in the department of internal medicine at Steve Biko Academic Hospital in Pretoria.