Featured Item

Netcare chief calls for stricter lockdown measures in Gauteng
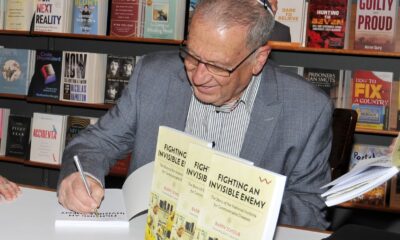
“It’s horrific out there,” said Dr Richard Friedland, the chief executive officer of Netcare, the country’s largest private hospital group, as rising COVID-19 infections continue to have Gauteng in a chokehold.
Friedland has called for urgent stricter lockdown measures in the province.
Earlier this week, he called for Gauteng to be placed under Level 5 lockdown. At the time of going to press on Wednesday, he said it was “critical” for people to self-regulate.
“I was hoping for a Level 5 lockdown in Gauteng. In its absence, I’m calling for much stricter and more strenuous lockdown measures. Schools should be closed, people should avoid all gatherings, and do online shopping where possible,” he told the SA Jewish Report.
“The bottom line is, it’s horrific out there. We are seeing a massive surge and significant volumes, which are threatening hospitals across the province.
“Some would argue it’s too late for harsher lockdown measures, and that the horse has already bolted. I’m saying there’s still time to prevent people from requiring hospitalisation,” he said.
Understanding the severe implications that lockdown measures have on the economy, he said, “Every soul, every life is precious, we have to do whatever we can to prevent further loss of life.”
According to forecasts, the Western Cape could face the same Gauteng wave in three to four weeks.
The Chevrah Kadisha is experiencing a significant increase in the number of deaths in the community.
Top health professionals have called for much stricter lockdown measures, while others have called for the vaccine rollout to pick up speed dramatically. Deputy Health Minister Dr Joe Phaahla said this week that registration for those 50 and older will open up on the Electronic Vaccination Data System in the coming days.
This is a vast unfolding tragedy as endless stories of hope and despair engulf the province during the devastating third wave.
Saul Tomson, the chief executive of the Chevrah Kadisha, said it was still premature to compare the numbers of deaths per wave because the province was still in the midst of the wave.
“We are extremely concerned given the high death rate, and the effects we are seeing on the community,” Tomson said. “It is too early to make statistical deductions on the third wave, but once again we have multiple teams working around the clock.”
He said the cemetery staff are working with incredible commitment and sensitivity. “Despite the intense pressure we need to ensure we continue to deal with every situation with kindness, compassion and professionalism.”
Professor Lucille Blumberg of the National Institute for Communicable Diseases has called for the vaccine rollout to move “much faster”.
“The vaccination sites are working efficiently, we have the capacity, we just need to move them out much quicker,” she said,
“Vaccines save lives, livelihoods, and will protect our health system,” she urged this week.
The healthcare system is fast becoming overwhelmed, and hospitals are struggling to cope as critical drugs and oxygen supplies are threatened with diminishing supply, say several doctors.
“What stands out for me is the sheer numbers of those affected and the spread in our community. We are drowning,” said Uriel Rosen, the operations manager and head of the Wellness Programme at Hatzolah.
At the time of going to press, the Hatzolah Wellness Programme had registered 329 new cases so far this week. There are 837 active cases, and 76 patients are on home oxygen.
The statistics show that 20% of active cases involve people under 20 years old; 22.5% of cases involve those between the ages of 20 to 40; 29% of cases involve those between the ages of 40 to 60; and 28% of cases involve those 60 years and older.
“We had 100 new cases on Tuesday alone,” said Hatzolah paramedic Yudi Singer.
He said the biggest frustration was trying to get severely ill patients admitted to hospital.
“There is a shortage of beds, and there is just so much we can do. It’s so hard when we have tried everything and we know the patient urgently requires hospitalisation and specialised care,” he said.
“These are very trying and challenging times. It’s tough on our teams, they are seeing death and seeing the health system taking strain. It’s heartbreaking for paramedics to see their patient’s name on the Chevrah Kadisha list after they have formed a special relationship with them and their family,” he said.
The Hatzolah team somehow makes sure each patient requiring hospitalisation is admitted, said Rosen. “Even if it means paramedics have to wait up to four hours with a patient in an ambulance outside the hospital.
“We’re in crisis mode, the hospitals are full, and patients are really sick. We are tired, but we are pushing through. Every volunteer, responder, and dispatcher is 100% committed to saving lives and making a difference. It’s all hands on deck.”
He said the virus was spreading far quicker within the family, with entire families affected.
Worryingly, he said some patients continued to deteriorate towards the end of their isolation period. “This isn’t evidence based, but we are seeing patients deteriorate later, sometimes from day 10.
“It’s comforting to know we are actively saving lives. We are picking things up early, which can and does significantly change an outcome,” he said.
Dr Carron Zinman of Netcare Linksfield Hospital said at the weekend she was literally examining patients who couldn’t be taken off oxygen in the back of ambulances.
“All beds at one stage were occupied in casualty. On Sunday alone, my partner and I saw 131 patients. Ambulances were parked outside with very sick patients needing oxygen.
“On Tuesday morning, we received 67 patients, 60 of whom had COVID-19. By 10:00, six of them had been intubated. I never dreamt of anything like this. In every wave I think we’ve seen the worst, then it surprises me,” she said.
“The moments that stand out for me is when a patient is about to be intubated. Seeing them make what could be their last phone call to their loved one is gut wrenching.”
There are multiple stories of pain and suffering. One patient was seen talking to his undertaker making his own funeral arrangements because he didn’t want to burden his family following his death.
One woman contracted COVID-19 during her pregnancy, and managed to deliver her baby successfully by C-section. “She was doing well, and then she arrested and later died. They spent 45 minutes trying to resuscitate her. It’s been 16 months fighting for people’s lives. For some nurses, this was the last straw,” she said.
Equally there’s jubilation when a very sick patient is successfully resuscitated and later discharged, Zinman said. Patients who have been vaccinated are also recovering faster. “We celebrate the victories,” she said.
Blumberg recognised the extraordinary service and support for the community by general practitioners, physicians, and especially Hatzolah, which she said had “established a remarkable programme”.