
OpEds

What you need to know about vaccinations
In the first week of the national COVID-19 vaccine rollout, more than 117 000 people were vaccinated, with many of our senior citizens receiving their first dose of the Pfizer vaccine. Gratifyingly, many residential facilities for the elderly, the most vulnerable of the vulnerable, were successfully vaccinated. Families are breathing collective sighs of relief, some even celebrating their perceived immunity. Do I really still need to wear a mask and take COVID-19 precautions?
Here are key examples of the questions I have been asked over the past week.
1. Does being vaccinated mean that I can now dispense with COVID-19 precautions? Unequivocally not. All the COVID-19 precautionary measures must still be strictly adhered to for several reasons. First, the immune response elicited by the vaccine will kick in about two weeks after vaccination but is really properly effective only after four weeks. Second – and very importantly – no vaccine is 100% effective. The effectiveness of the Pfizer vaccine against the dominant South African variant, B.1.351, is projected to be about 65% for mild or moderate illness and 85% for severe illness. In other words, the chance of still getting mild or moderate illness is about 65% lower, and for severe illness about 85% lower, compared to unvaccinated individuals. If not careful with precautions, there still remains significant risk of infection and illness, from mild to severe. We will be able to return to our pre-COVID-19 life only once herd immunity has been reached and the circulation of the virus has been controlled.
2. If I have had COVID-19 previously, do I still need to be vaccinated? Definitely. Because more than 95% of virus strains in South Africa are of the relatively immune-resistant B.1.351 variant, high levels of neutralising antibodies are needed for protection. These levels are often not reached by natural infection. The COVID-19 vaccines being used in South Africa – Pfizer and Johnson & Johnson – have been very cleverly engineered to produce an even more powerful stimulation of the immune system than occurs with natural infection.
3. Why does the Pfizer vaccine require two doses while Johnson & Johnson only requires one? These two strategies have followed from their respective clinical trials. The Johnson & Johnson vaccine has been shown to retain a very strong immune response for many months after a single dose, while the strong immune response with Pfizer was seen after the second dose.
4. If I have been vaccinated and come into contact with an infected person, must I still quarantine for 10 days? Yes – the same as if you weren’t vaccinated. As mentioned above, you could still be infected, and even if not showing any symptoms, you could still pass on the infection.
5. If I’m not feeling entirely well, should I still keep my vaccination appointment or postpone it until feeling absolutely fine? This is a little tricky. If symptoms are suggestive of COVID-19, you should be tested rather than go for vaccination. However, if they are mild and not suggestive of COVID-19, there should be no reason to postpone a vaccination appointment.
6. If I have recovered from a bout of COVID-19, how long should I wait before being vaccinated? Four weeks.
7. The recommended interval between the first and second doses of Pfizer in the United States (US) is three weeks. Why are we recommending a six-week interval? Clinical trials of the Pfizer vaccine were carried out with a three-week interval, and consequently US regulatory authorities have maintained that recommendation. However, the United Kingdom (UK) decided to extend the interval to 12 weeks, primarily to vaccinate and provide some degree of protection to as many as possible with at least one dose. An added advantage was that the longer interval produced a stronger immune response than the three-week interval, something also observed with many other vaccines. We have taken a middle path, in concert with the World Health Organization, to delay for six weeks for an enhanced immune response but not as long as the UK recommendation out of concern about people neglecting or forgetting about the second dose.
8. Should I do an antibody test after vaccination to confirm that I have immunity? This isn’t recommended by international bodies such as the US Food and Drug Administration. Routine antibody tests are unreliable in establishing immunity (although they may have a role in determining whether someone has previously been infected).
9. What side effects can I expect from the vaccine? Most people won’t experience any side effects. Some may have tenderness or a rash at the injection site. Occasionally, for a day or two, rarely longer, there may be some headache, feeling out of sorts, some muscle pain, or even a slight fever, which could be controlled with something like Panado. Any more serious adverse event must be reported to a medical practitioner for onward transmission to the NISEC (National Immunisation Safety Expert Committee). Alternately it can be reported through the “MedSafety” app.
10. If I’m an allergic type of individual (previous vaccination or medication, foods, pets, grass, etc.) should I get vaccinated? Severe allergic reactions (anaphylaxis) to the Pfizer vaccine have been reported, but these have been extremely rare – calculated at 11 per million doses. About three quarters of these have occurred within 15 minutes of vaccination. It would therefore be important for allergic individuals to alert the staff doing vaccinations, and one should wait for 30 minutes instead of the usual 15 minutes after vaccination. The risk of blood clots after the Johnson & Johnson vaccine is less than one per million doses and has not, to date, been reported after the Pfizer vaccine.
11. A frequent question about vaccination comes from patients with various chronic underlying medical conditions. In the first instance, this should be discussed with the attending doctor. In broadly general terms, the COVID-19 vaccine can be given – and in most of these cases should be given – to persons with underlying medical conditions, especially where the immune system may be suppressed by illness or chemotherapy. But this must be discussed with the attending doctor.
12. If I have had the influenza vaccine or any other vaccine, how long should I wait before getting the COVID-19 vaccine? We recommend a waiting period of at least two weeks to minimise the mild-side reactions mentioned above.
In conclusion, I reiterate that both vaccines, Pfizer and Johnson & Johnson, are safe and highly effective. There is nothing to choose between them, and the advice is to take whichever vaccine is offered first in order to be vaccinated as soon as possible. Advice and recommendations will change from time to time as more and more is learnt about this new disease and newer vaccines are developed to prevent it. Importantly, advice must always be sought from authentic, reputable sources.
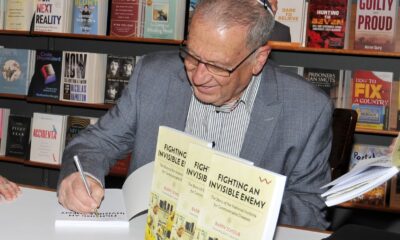
- Barry Schoub is the chairperson of the Ministerial Advisory Committee on COVID-19 vaccines. He is the founding director of the National Institute for Communicable Diseases, and professor emeritus of virology at the University of the Witwatersrand. He isn’t employed by the department of health, receives no remuneration from the department, and isn’t a spokesperson for the department.










Jackie
May 27, 2021 at 11:01 am
Thanks for the info. Do you need to re-registet with EVDS, for second Pfizer shot?
Loretta Barnett
May 27, 2021 at 1:16 pm
My husband & I both in mid, & late eighties drove to Michells Plain Lenteguer clinic to be vaccinated. Everything went well & fine…….. till drive home. We got terribly lost in very bad area.
My question is, we live in SEA Point Fresnaye area, the next one is due in 3 weekstime. Will we please be able to have it nearer home for fear of getting lost again?
Thank you